(Credit: Bigstock)
(Credit: Bigstock)
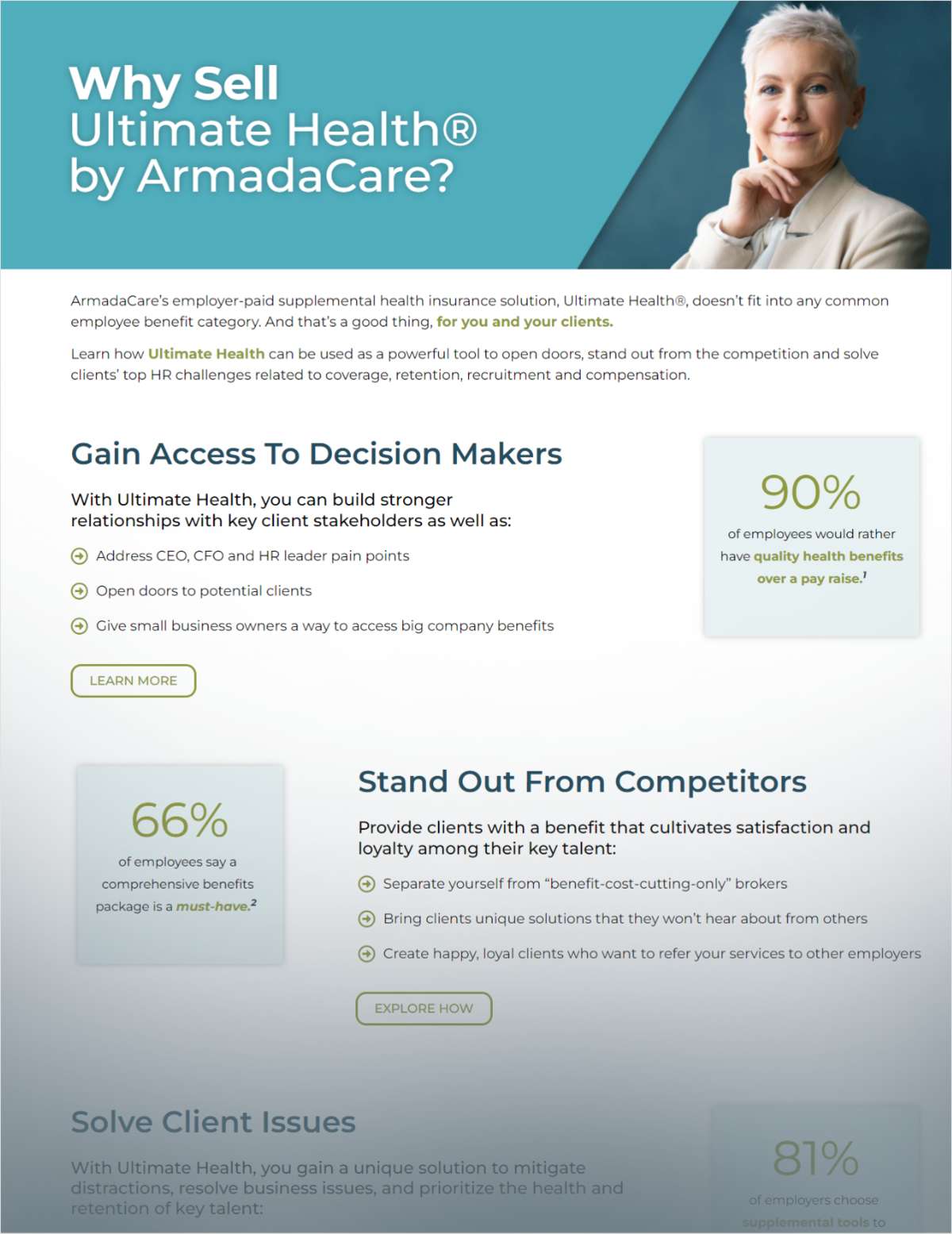
Medicaid has helped level the health care playing field for people of color, especially during the pandemic. Promoting continuity of coverage as states unwind the Medicaid continuous enrollment provision can continue to help mitigate disparities in coverage and care, according to a new report from KFF.
The Families First Coronavirus Response Act included a temporary requirement that Medicaid programs keep people continuously enrolled in the exchange for enhanced federal funding. However, this provision ended in March, and states will need to conduct redeterminations for all Medicaid enrollees during the next 12 to 14 months. An estimated 17 million people could lose Medicaid coverage, and research shows that Hispanic and black people are likely to be disproportionately affected.
Complete your profile to continue reading and get FREE access to BenefitsPRO, part of your ALM digital membership.
Your access to unlimited BenefitsPRO content isn’t changing.
Once you are an ALM digital member, you’ll receive:
- Critical BenefitsPRO information including cutting edge post-reform success strategies, access to educational webcasts and videos, resources from industry leaders, and informative Newsletters.
- Exclusive discounts on ALM, BenefitsPRO magazine and BenefitsPRO.com events
- Access to other award-winning ALM websites including ThinkAdvisor.com and Law.com
Already have an account? Sign In
© 2024 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.