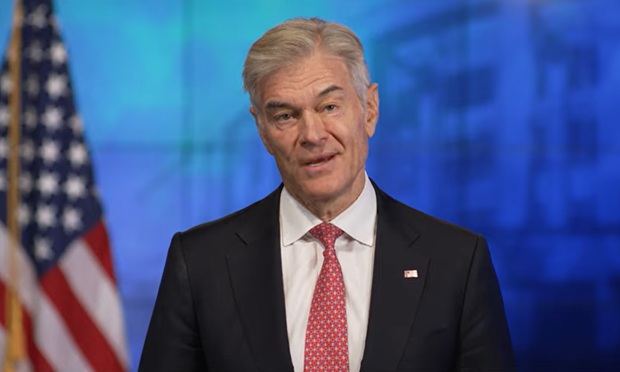
 Dr. Mehmet Oz. Credit: CMSHHSGov
Dr. Mehmet Oz. Credit: CMSHHSGov
Dr. Mehmet Oz — now the administrator of the Centers for Medicare and Medicaid Services — is starting off by talking about improving health care system integrity.
"One of my first priorities is going to be to crush fraud, waste, and abuse," Oz said in a video posted Thursday on the CMS YouTube channel. "I'm going to have more news on that coming soon."
Recommended For You
In a list of health policy priorities posted on the CMS webite, Oz cited the need to help patients find out what their care will cost, to protect health care providers against unnecessary paperwork and to modernize the Affordable Care Act public exchange program.
Oz did not say anything about employee health benefits or workers' health.
The Senate confirmed the surgeon and former TV talk show host as the CMS administrator April 4.
Related: Senate confirms Dr. Oz as CMS administrator on a party-line vote
CMS is the U.S. Department of Health and Human Services agency that runs Medicare and Medicaid.
CMS also works with the Employee Benefits Security Administration, a U.S. Labor Department agency, and the Internal Revenue Service to oversee the Affordable Care Act rules and programs that affect commercial health insurance, such as HealthCare.gov, the ACA essential health benefits package and the ACA employer health coverage requirements.
One reason for the lack of discussion about group health coverage and employee benefits may be that Oz is still waiting for the Senate to confirm the assistant Labor secretary who will serve as the head of EBSA.
President Donald Trump nominated Daniel Aronowitz, an ERISA law expert who runs a company that provides insurance for benefit plan fiduciaries, to the top EBSA post in March.
At press time, Senate committees had not scheduled any confirmation hearings for Aronowitz, and the U.S. Office of Government Ethics had not posted his financial disclosure document.
Oz's remarks about fraud, waste and abuse could be a sign that he'll be moving ahead with ideas he discussed at a Senate confirmation hearing in March about easing providers' problems with health plans' procedures for authorizing coverage for care.
Oz suggested that one way to help providers cope would be to create a relatively short, standardized list of procedures that may be subject to prior authorization review.
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.







