 The implementation of the Patient Protection and Affordable Care Act has made most employers “rethink” their employee benefit offerings, including increasing employees' share of cost even more via consumer-driven plans.
The implementation of the Patient Protection and Affordable Care Act has made most employers “rethink” their employee benefit offerings, including increasing employees' share of cost even more via consumer-driven plans.
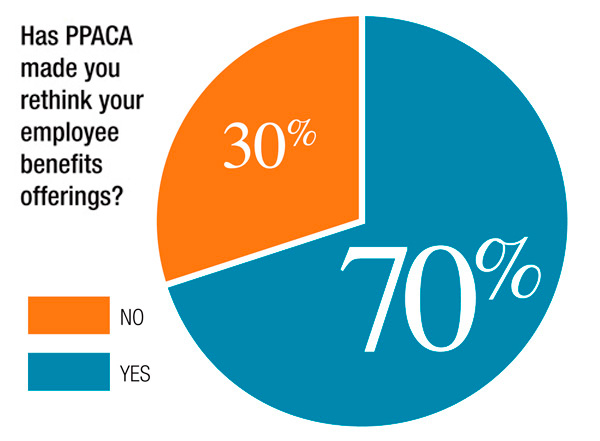
According to Benefits Selling's 2014 Employer Survey, 70 percent of employers said PPACA has made them rethink their employee benefit offerings, compared to 30 percent who said the health care reform law hadn't had any impact on their offerings.
“PPACA definitely changed the way we think about benefits, to the point that we're actually implementing a marketplace exchange, using Aon's exchange,” says survey respondent Maggie Peabody, benefit analyst at Orica, an Australia manufacturing and mining company with global operations. Peabody is based in Watkins, Colorado.
Recommended For You
Complete your profile to continue reading and get FREE access to BenefitsPRO, part of your ALM digital membership.
Your access to unlimited BenefitsPRO content isn’t changing.
Once you are an ALM digital member, you’ll receive:
- Breaking benefits news and analysis, on-site and via our newsletters and custom alerts
- Educational webcasts, white papers, and ebooks from industry thought leaders
- Critical converage of the property casualty insurance and financial advisory markets on our other ALM sites, PropertyCasualty360 and ThinkAdvisor
Already have an account? Sign In Now
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.








