In the self-insured world, “centers of excellence” is a term that is beginning to be used for a specific hospital that has been selected by a large employer for bundled pricing of high-ticket, higher-volume surgeries like knee replacement.
The label alone heightens expectations of vastly superior health care. Consumers want to believe they will experience care that is off the charts in all respects; from advanced techniques, expedited treatment and length of stay, to pain management and overall patient satisfaction.
The name implies that centers of excellence (COEs) are somewhat immune to the inherent dangers of hospitalization. This expectation persists, despite a recent study estimating that a quarter of a million deaths are caused by medical errors each year.
The assumption most employees have about COEs is that they are first and foremost selected based on performance; that objective measures of outcomes like mortality and complications are top selection criteria. They expect that only after the performance quality is determined are prices taken into consideration to find the best value. They assume that centers of excellence live at the intersection of amazing quality and good price.
Rise in popularity
With the rapid increase in cost of health care over the last decade, self-insured employers have sought out lower cost structures by engaging directly with hospitals. This trend is a big part of what is driving the popularity of COEs.
These are typically hospitals with great name recognition that contract directly with self-insured employers to provide fantastic deals for paying cash or expedited payment terms. The hospital is happy because they improve their cash flow (bypassing insurance companies whose payments are often delayed by months), employers are happy because they are often paying less money, and the employees are happy because they believe they are going to a place that has been vetted as “the best of the best.” On the surface, it seems everybody wins.
Lack of outcomes transparency
Unfortunately, trustworthy outcomes-based metrics have not been widely available until recently, so as a proxy for excellence, employers have had no alternative but to identify top providers based on name recognition and reputation.
With this in mind, our analytics team set out to investigate whether centers of excellence truly provide exceptional care. We tackled this problem by analyzing the outcome metrics for existing COEs.
While most of these centers have great national reputations, the data show surprising areas of mediocre and even poor performance. This included high variance in hospital outcomes across the different procedures performed; for example, a hospital can be exceptional at hip replacement, but nowhere near as good for heart bypass surgery.
We would not go as far as to say there is no correlation between reputation and outcomes, but more often than not, one does not guarantee the other.
We also found surprisingly little evidence supporting the assumption that outcomes are the top driver of COE selection. In fact, it would appear that the top factors that drive selection are price and reputation. In other words, centers of excellence are always “excellent” in pricing, but not necessarily “excellent” at performance.
The cost of poor quality
So should self-insured employers care about quality? Why upset the apple cart if no one is complaining?
If a quarter of a million deaths from medical errors isn't enough of a reason to care about quality, how about the fact that poor health care quality costs payers hundreds of billions of dollars a year?
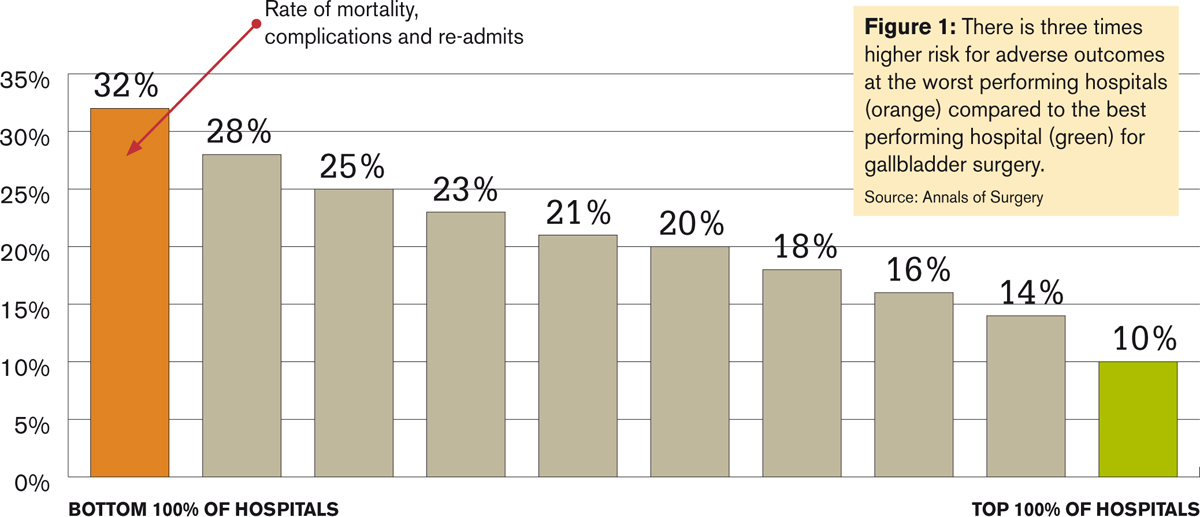
A series of studies conducted recently by MPA Healthcare Solutions in Chicago showed that poor performing providers pose two times greater risk of adverse outcomes (such as severe complications or mortality) in colon and cardiac surgery, and three times greater risk of adverse outcomes in gall bladder surgery, hip, knee, kidney removal, and lung resection surgery.
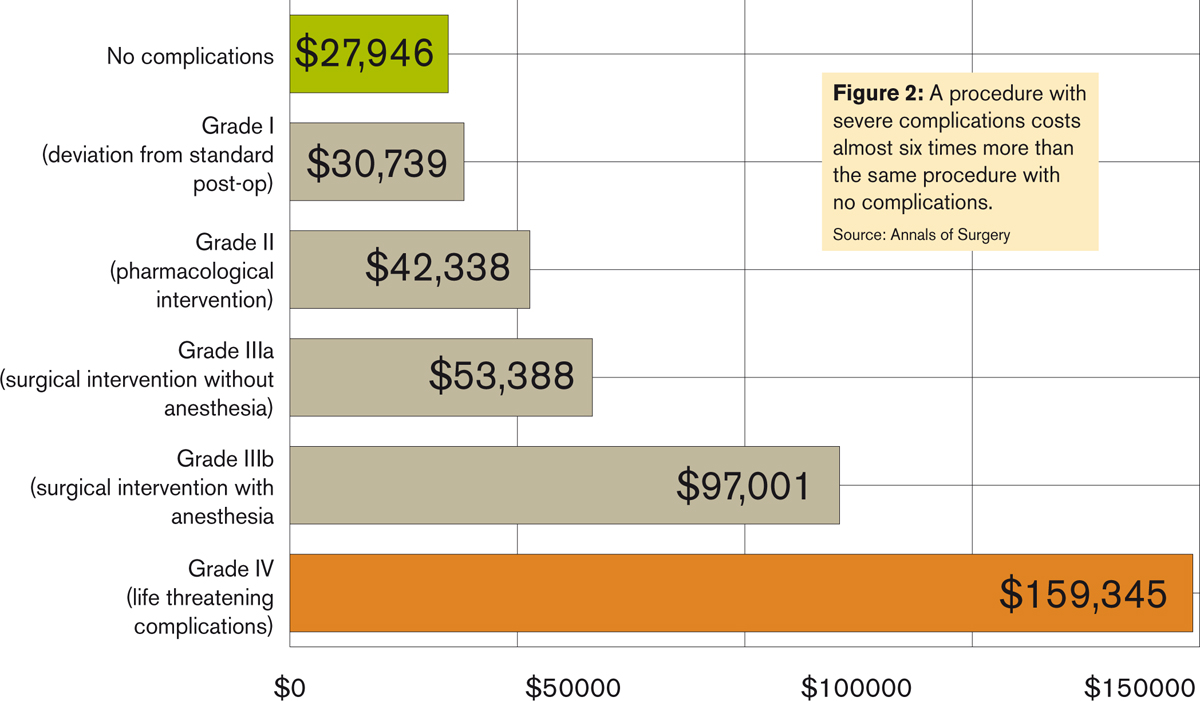
Complications lead to extended hospital stays and readmissions, and ultimately translate to higher costs and more suffering for patients. In a 2011 study published in the Annals of Surgery, the investigators found that a procedure resulting in severe complications costs nearly six times more than the same procedure with no complications.
That well-negotiated $18,000 sticker price on knee surgery, which saved a self-insured employer $10,000 upfront, has the potential of quickly turning into $100,000 if a major complication occurs, and this does not take into account the indirect costs of lost productivity, not to mention unnecessary patient suffering.
The search for quality
It's clear that the term “center of excellence” needs to be redefined. Here are the five critical steps to truly achieve excellence.
1. Ruthlessly ignore reputation
The first step in selecting better centers of excellence is to put your preconceptions aside and become reputation agnostic. As noted, reputation does not always correlate to quality. Case in point: A Chicago hospital, touted as a “nationally recognized leader” according to their website, was recently selected by a very large self-insured employer as a center of excellence for knee and hip surgery.
The hospital's orthopedic department is considered “#1 in all parts of Chicago,” which is presumably what helped them become a center of excellence to great fanfare.
Unfortunately, three continuous years of outcomes data does not support the hospital's reputation. When examining risk-adjusted severe complications and overall adverse outcomes, the above referenced hospital ranks far below the national average of performance for orthopedics providers in the country.
When it comes to knee and hip replacement surgery, it performed at the absolute bottom. In terms of long-term clinical outcomes for these procedures, on a 100 to 800 point scale, their quality scores for both procedures are at the poorest performance of 100.
To further illustrate how reputation doesn't matter, one of the best hospitals in the country for knee replacement surgery is an all but unknown facility — Valley Baptist in Harlingen, Texas. Yet, despite lacking a national brand name, Valley Baptist has performed at the absolute top on the scale with a score of 800. As these examples show, one should heavily discount reputation as part of a center of excellence selection.
2. Medical quality analytics: Don't do it yourself
Unless you're a surgeon with a PhD in statistical analysis and a decade or two of experience grappling with medical performance data, you need to find a team to perform the due diligence necessary to evaluate whether a hospital is performing well.
With some digging, an experienced health care analytics team would be able to direct a self-insured employer from the above mentioned reputable-but-poorly-performing Chicago hospital, to the equally reputable but demonstrably high-performing Northwestern Medicine Network, including hospitals in the Greater Chicago area like Central Dupage in Winfield with a score of 710 in knee replacement surgery and Lake Forest Hospital with a score of 610 in hip replacement surgery.
One of the biggest pitfalls we see with self-insured employers is the outsourcing of due diligence to organizations — including employer coalitions — lacking health care analytics or statistics capabilities. If you wish to pursue the center of excellence model, it's important to qualify the team and find people, organizations or platforms that incorporate strong health care analytics experience.
3. Outcomes, outcomes, outcomes
The most important step in selecting true centers of excellence is to focus on objective outcomes. Objective outcomes are metrics that are measurable and not biased by perception. For example, mortality is an objective outcome. Complication rate is an objective outcome. Readmission rate is an objective outcome.
By contrast, patient satisfaction is not an objective outcome, because “satisfaction” is colored by things that do not meaningfully contribute to health care results. In fact, there has been evidence that shows that subjective outcomes like patient satisfaction are inversely correlated with effective patient care.
With the 2013 and 2014 releases of massive Medicare provider data, there is at least one publicly available data set for looking at outcomes, and there are now a handful of analytics efforts ranking and scoring the various hospitals based on these raw data sources.
Importantly, when you look at health care quality metrics, make sure that whatever platform or methodology you choose, there is risk adjustment for the patient population (meaning, hospitals with sicker patients are not penalized for taking on those patients). Also, you must scrub the raw data and normalize it against facility variations, and you must have robust statistical weighting to ensure a truly comparable rating system.
4. Look for cost effectiveness
You can stop at step three if you like, because outcomes-based quality is the minimum standard for selecting a center of excellence. However, for most self-insured companies, lowering health care cost is a major motivator. To this end, a filter based on cost can be applied to find the best providers with the lowest cost as a final step. You can take your list of excellent providers and your table of costs for each procedure and map them to one another.
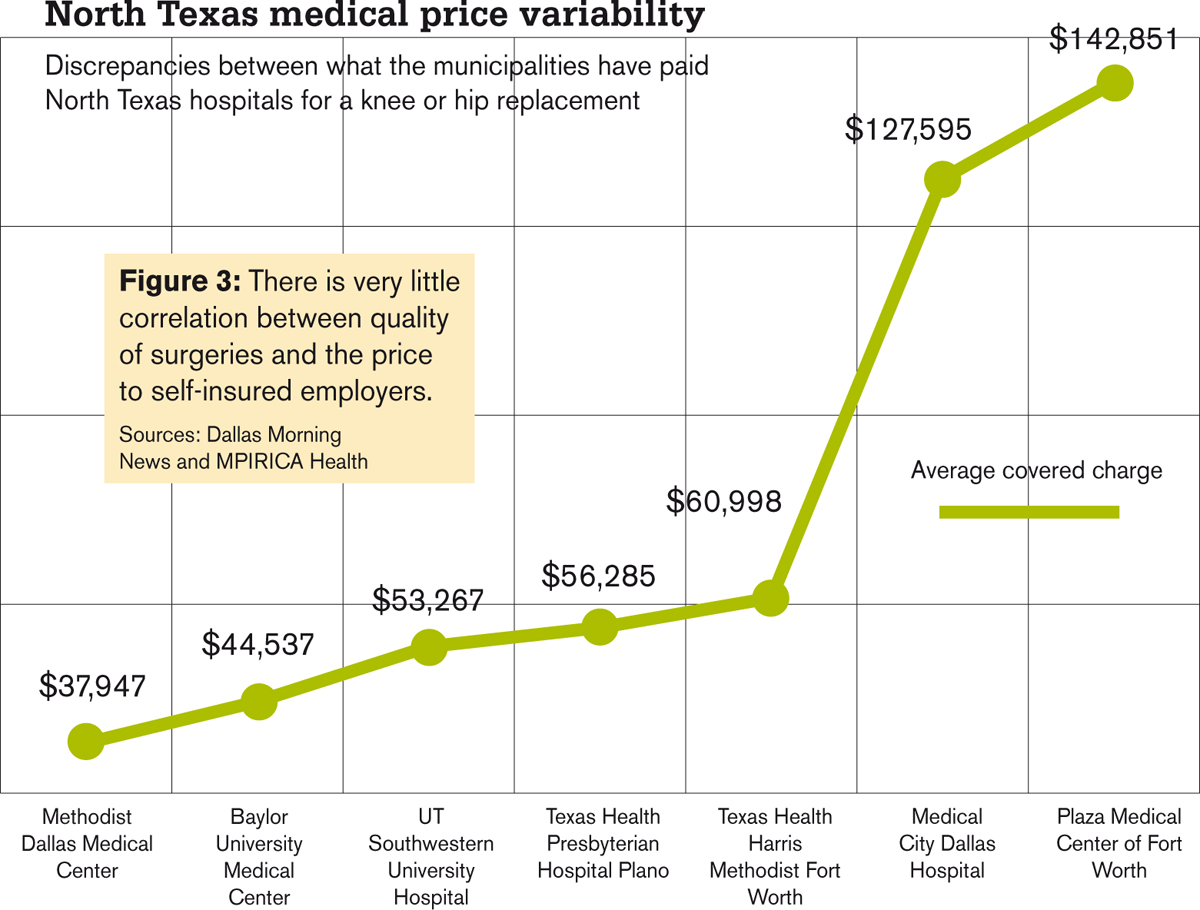
Now, if you think low cost and high quality are mutually exclusive, think again. As noted earlier, lower quality actually costs more money because of longer hospital stays and more medical intervention. While health care costs can be complex, just looking at the orthopedics price data from North Texas as reported in the Dallas Morning News, combined with knee replacement quality scores, you can see that the lowest cost hospitals are amongst the highest quality providers in the group.
5. Direct procurement
Once you establish quality and find value, the final step is to engage with the hospital organization to establish a relationship for direct procurement of services.
The core tenet of a center of excellence model is negotiating a relationship that is a win-win for both the provider and self-insured employer. The key features of the relationship should include reference-based bundled price, fast cash payment and quality monitoring.
These relationships encourage ongoing quality and efficiency from the hospital, and allows the employer to steer patients to the provider by offering incentives like zero out-of-pocket costs or cash back.
The take-home message
Finding and contracting with a center of excellence for specific procedures is a great way to lower costs for self-insured employers, but it takes a bit of legwork.
However, if you follow the steps laid out above, you will be able to take advantage of the COE trend, save money, and protect your most important asset: your employees. This is what a true win for everyone looks like.
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.







