Insurance-industry groups said Wednesday that they oppose a Republican proposal to repeal and replace the Affordable Care Act, joining health-care providers in asking Senators to reject the bill.
America’s Health Insurance Plans and the Blue Cross Blue Shield Association said they oppose the plan, backed by Republican Senators Lindsey Graham, Bill Cassidy, Dean Heller and Ron Johnson, because it would make it harder for individuals to get coverage and cut funding for Medicaid. In addition, unlike previous repeal attempts, the bill would leave a tax on health insurers in place.
The bill “would have real consequences on consumers and patients by further destabilizing the individual market; cutting Medicaid; pulling back on protections for pre-existing conditions,” AHIP said in its letter. The group said the GOP plan would backfire, “potentially allowing government-controlled single payer health care to grow.”
The plan would cut U.S. spending on the Affordable Care Act’s expansion of health coverage by about $81.6 billion through 2026, according to an analysis by consultancy Manatt Health. When the bill’s caps on the broader Medicaid program are included, spending would drop by $215 billion, according to consulting firm Avalere.
The analyses and industry opposition present more obstacles for the renewed push to undo the Affordable Care Act ahead of a Sept. 30 legislative deadline. Late Tuesday, the talk-show host Jimmy Kimmel, whose emotional appeal helped crystallize opposition to an earlier repeal-and-replace bill, told viewers to oppose the new legislation. Kimmel said Cassidy, a medical doctor from Louisiana, lied when he previously promised on Kimmel’s program that any health overhaul would protect sick children.
“I’m sorry he doesn’t understand,” Cassidy said in an interview on CNN on Wednesday. “More people will have coverage, and we protect people with pre-existing conditions.” Cassidy said his law would have the same protections for sick people as Obamacare.
Broadly, the Graham-Cassidy bill keeps most of Obamacare’s taxes, while undoing the law’s insurance expansion and redirecting the funds to states as block grants. That would give the states broad discretion over how to use the funds. At least 20 million people have gained insurance coverage under Obamacare, mainly through the expansion of the Medicaid program to more low-income people.
The bill has drawn opposition from a broad swath of health-care groups, including the American Medical Association and the American Hospital Association. The groups largely backed Obamacare and opposed previous repeal attempts.
“We believe the Graham-Cassidy Amendment would result in millions of Americans losing their health insurance coverage, destabilize health insurance markets, and decrease access to affordable coverage and care,” the AMA said.
The nonpartisan Congressional Budget Office, which evaluates legislation for lawmakers, has said it won’t have time to evaluate the full effects of the repeal plan before a potential vote next week. CBO said it plans to publish a more limited analysis by early next week.
Neither of the consultant reports estimated how many people overall could lose insurance coverage.
The flexibility granted to the states could allow them to set up markets where individuals who have so-called pre-existing conditions are charged more for insurance than others, according to the Manatt analysis. States could also potentially remove other pieces of the ACA’s insurance regulations, including requirements that health plans cover essential health benefits, such as prescription drugs, hospitalization, and maternity care.
“In states that obtain waivers, individuals with pre-existing conditions could face substantially higher premiums in the individual and small group markets, or find their policies do not cover essential services,” according to the Manatt analysis.
Because the bill depends on states to implement it, the exact effects on coverage are difficult to estimate. Manatt said that over the 2020-2026 period, when the bill is designed to go into effect, 29 states would receive less federal funding than under Obamacare, with an average cut of 19 percent. The funding ends after 2026, creating a severe dropoff in health-care payments, though supporters of the law have said it would be reauthorized.
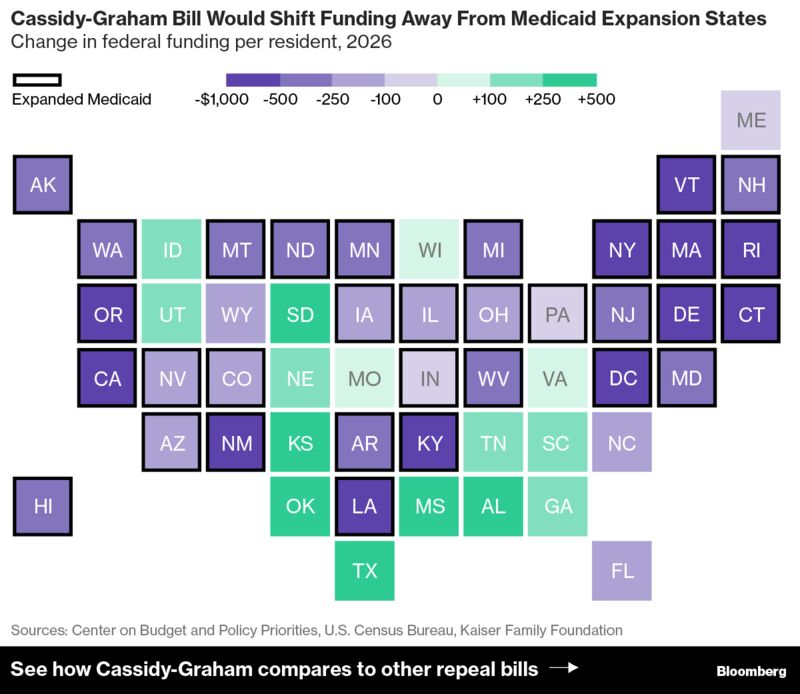
The analysis from Avalere finds that when the broader Medicaid cuts are taken into account, 34 states and the District of Columbia would see reductions in federal funding over the 2020 to 2026 period, while 16 would gain. The Avalere analysis was funded by the left-leaning Center for American Progress.
Recommended For You
Conservative criticism
Republican lawmakers have been pledging to repeal and replace Obamacare since it was signed into law in 2010, but some right-leaning groups have been lukewarm on the Graham-Cassidy approach because it leaves much of the law’s taxes in place.
FreedomWorks, an advocate for conservative causes, said it’s not yet taking a position.
“We don’t support nor do we oppose Graham-Cassidy,” the group said in a statement on Wednesday. “Although this amendment fails to meet more than seven years of promises to repeal ObamaCare and does not truly represent an approach grounded in the principles of federalism, there is a path to win our support.”
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.







