Many frustrated consumers simply throw away an explanation of benefits when it comes in the mail. (Photo: Shutterstock)
Many frustrated consumers simply throw away an explanation of benefits when it comes in the mail. (Photo: Shutterstock)
Transparency has been a key focus in the effort to create better health care consumers. But as employers try to help them understand the relationship between medical costs and health insurance premiums, one area that needs a little more explanation is, well, the explanation of benefits.
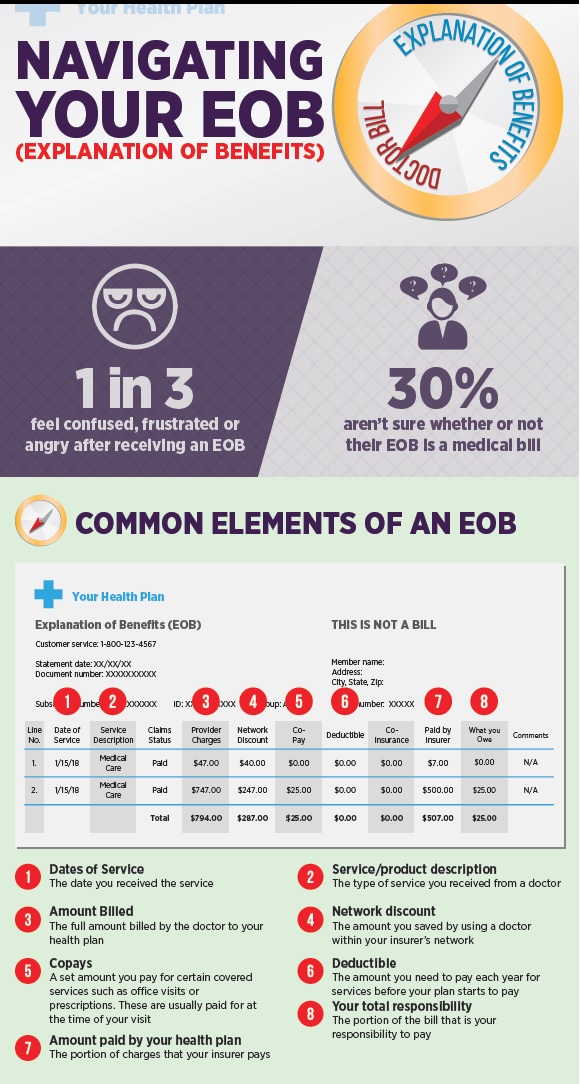
According to a recent survey from Vitals, an online resource for health care transparency, for one in three consumers, the arrival of an EOB in the mail (or digitally) causes confusion or frustration, and they're unsure what the dollar amounts on the EOB mean–and who is going to pay them.
Recommended For You
"Contrary to popular belief, high-deductibles and health savings accounts (HSAs) alone won't create empowered health care consumers or functional health care marketplaces," said Mitch Rothschild, founder and chairman of Vitals. "Stakeholders across the health care ecosystem need to innovate, remove friction points and design products and processes that are easy-to-use, convenient and value-priced."
According to Vitals, part of the problem is a lack of industry standards with regard to creating an EOB. Without a confident understanding of what the codes or procedure names mean, patients are unsure how to read the bill, which, in turn, leads to apathy, according to the research, with one out of 10 consumers surveyed admitting that they typically throw out the EOB.
However, as the push for greater transparency has shown, consumers are doing themselves and their health insurer a disservice. Auditors have found that more than 90 percent of the hospital bills contain an error, resulting in significant overcharges.
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.