 I recently received both glares and head nods in a leadership meeting with competitors, hosted by a national carrier, after I said “Over the past decade, I don't think any other industry has been more excited than ours about 97 percent adoption rates, and 3 percent utilization rates. Employers want something that works.”
I recently received both glares and head nods in a leadership meeting with competitors, hosted by a national carrier, after I said “Over the past decade, I don't think any other industry has been more excited than ours about 97 percent adoption rates, and 3 percent utilization rates. Employers want something that works.”
History and health literacy
Somewhere in the late 1990s, the continued upward trend in health insurance costs paved the way for “consumer-driven health plans” (CDHPs). The question is, have CDHPs been ahead of their time with the notion that educated consumers could pave the way to create change, without the tools, resources, or transparency to do so effectively?
By 2003, CDHPs received a lift with the creation of health Savings Accounts (HSAs). By 2007, roughly 5 percent of those who secure coverage through their employer were enrolled in a consumer-driven plan; however, less than a decade later, it had risen nearly six-fold to 29 percent, according to the Kaiser Family Foundation.
The jury is still out on whether we can truly call these plans “consumer-driven health plans” when the medical industry is far from forthcoming with the tools or transparency needed to be a good consumer. But that's a conversation for another day.
Many believe that true transparency is an ideal destination for solving our nation's health care woes; however, I am more skeptical and see it as a waypoint along the longer journey. The U.S. Department of Education, Institute of Education Sciences provided data in 2003 as a part of a National Assessment of Adult Literacy, that only 12 percent of Americans were proficient in health literacy – that's roughly 1 in 8 Americans. Health plans have also increased in complexity, making it even more challenging.
QUESTION: Can one effectively navigate cost and quality and advocate for one's self, in order to best determine who should have a piece of their health care dollar, if 7 out of 8 may lack the tools, resources, or understanding needed in order to effectively do so?
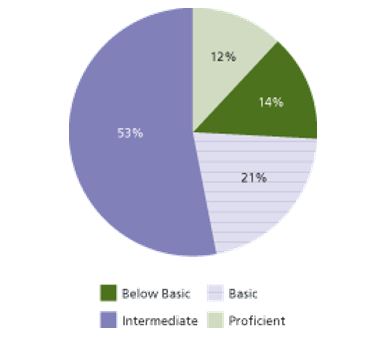
Source: https://health.gov/communication/literacy/issuebrief/
Patient/consumer (aka, you)
It is equally as important to note that this shift starting in the 1990s had other unintended consequences. As more cost burden shifted to patients as a means to help control costs, doctors and hospitals also had to make changes. The growth of administrative roles in health care also started to outpace doctors even more rapidly starting in 1990. Aggregation, legislation, documentation and, less cited but still important, billing and collections have all driven this growth.
The key question is, if health care is so confusing and burdensome that it takes a ratio of 10 administrators to every one doctor to manage, how can we expect consumers to do the same with the limited tools, resources, and transparency available on their side?
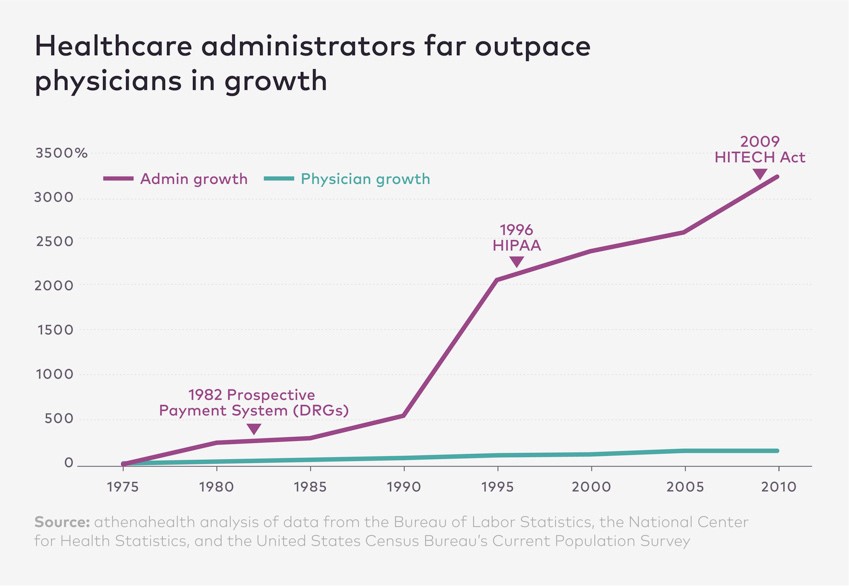
Source: https://www.athenahealth.com/insight/expert-forum-rise-and-rise-healthcare-administrator
What is “people-driven”?
Creating a plan with intention, in which the aim is to provide participating members with the tools, resources, advocacy, and human guidance they deserve, is where we see the clean break between legacy health plans and people-driven health plans.
If we look at the legacy health plan as being a three-legged stool between network, administrator/TPA, and PBM, a people-driven plan is a solid office chair on a swivel with the added support of a concierge. Not only can you pivot with ease, but also you can lean back and relax, knowing you have support.
One of the analogies I enjoy using is this: “When you are driving down the road with the aide of a navigation app, do you have the verbal turn-by-turn navigation turned on or off?” I still receive mixed answers to this, but overwhelmingly the guidance is turned on. I personally would rather know I missed my turn right away, rather than 10 miles down the road. The human voice (even when artificial in nature) is still powerful to hear.
By using an embedded concierge-style advocacy solution, members have the on-the-go ability to research provider quality, receive cost estimates, seek resolution to billing issues, and even be redirected to lower cost, higher performing providers, all with their own personal health care assistant on-call at the concierge advocacy solution.
Related: Creative plan design: from traditional to possible
Interestingly enough, the insurance industry net promoter score (which operates on a -100 to +100 point scale) is a 12; typically you can find a solid NPS of 80 and above for concierge solutions.
While telemedicine is still thought by many to be the savior that our health care system needs, I would beg to question how many other programs have 97 percent adoption rates, with 3 percent utilization rates (cough, EAPs; cough, wellness). Advocacy solutions can also lend a much-needed shot in the arm for many telemedicine programs as well, as a part of a well-rounded people-driven approach.
The results
We see results using concierge services in several key areas, ranging from cost reduction to increased member satisfaction.
A recent case study in the industry illustrated an average savings of $530 per contract, with a 65 percent increase in benefits knowledge, a 57 percent reduction in out-of-network costs, 90 fewer total ER visits per year, and 2.5 hours saved per member interaction.
In our own cases where an advocacy solution is embedded into the plan itself as a front-line defense mechanism, we are seeing an average savings yield on average of over $1,000 per utilizing household, and reduced claims issues as a result, since advocacy solutions can assist with keeping members in-network and avoiding surprise bills.
How do you do it?
Here are some easy tips to build a people-driven plan design, regardless of your current plan design:
- Integrate the right solution. A client and advisor should work closely together to understand the goals of the program, and back into the right fit to best integrate with not only the health plan, but also company culture. As time goes on, and should the opportunity arise, an advocacy solution can take on the entire service experience for the plan. A key question to ask in this process is how the advocacy solution promises to promote their solution to members, but also to solicit member feedback on what is most important to them.
- Remind, educate, engage. Staying top of mind is extremely important to ensure program success. It is unfair to think that dedicating five minutes during an hour-long benefits briefing once a year will provide results. Having a robust, year-round campaign, but also putting stopgaps in place (see below) can help to drive this home further and to help keep the solution relevant when it is needed the most.
- Consider incentives. Providing member incentives is much easier with an integrated solution. How does $0 for advanced imaging sound as a solution? By capturing advanced imaging and engaging members early in the process, we put both the member and the plan in a far better position of engagement as it relates to being a valuable solution in the course of treatment . This is especially true, given that MRIs, PETs, and CTs are often the gateway to more expensive care and treatment. Here is what I thought was a clever idea in the event anyone would like to recreate it.
- Stop-gaps. In an effort to capture as many cases as possible, having an advocacy solution embedded into your program can help to remind, incent, and drive utilization. These solutions can be triggered at the onset of a pre-certification or take the place of the benefits help desk.
- Set expectations. Ensuring that the right expectations are in place is the best medicine to ensure continued success. This means acknowledging early on that the solution is needed to help better support people-driven intent and continuing to promote the program at every turn, while also soliciting member feedback is all important for long-term success.
Key questions
For the skeptics, here are some questions to help consider if an advocacy solution can help you, your clients, or your people.
- Aside from showing if a doctor is in-network, does your health plan or network directory also show quality ratings? Accepting that a good first step is a network directory more like a Yellow Pages, and less like Yelp!.
- Does your health plan create an easy pathway for a member to receive accurate cost information to help better locate low-cost solutions for care? Many embedded solutions rely on historical third-party data from third-party tools and may not provide accurate ranges to rely on, assuming you can navigate through the clicks it takes from your health plan's home page.
- Does your health plan triangulate the results from the two questions above to locate the highest quality, lowest cost solution? This is my simple bash against transparency when 7 out of 8 Americans lack the understanding to make informed decisions. Health care operates in a vacuum of its own where, more often than not, the higher cost solutions correlate to the lowest quality solutions.
- When comparing quality metrics, is the information clinically based, crowdsourced, or non-existent? Not everyone is an acclaimed food critic, but they can still leave a review on Yelp!. The same applies to many of the health care research tools available. If you called your health plan to find the best-performing hospital in your network, would they help you to choose a higher quality option over a lower quality option, using data to back-up the recommendation?
Soapbox to solutions
Yes, I understand that much of this was a soapbox about an increasingly complex delivery system, in an era of rising healthcare costs, with decreasing member satisfaction. However, we truly believe that the shift from a legacy health plan to a people-driven health plan is what not only the industry, but also disenfranchised health plan members desperately need.
© Touchpoint Markets, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more inforrmation visit Asset & Logo Licensing.






