 If full-time, permanent workers who decline individual coverage HRAs end up qualifying for the ACA exchange plan premium tax credit, the employer could end up facing employer mandate penalty bills. (Image: Allison Bell/ALM)
If full-time, permanent workers who decline individual coverage HRAs end up qualifying for the ACA exchange plan premium tax credit, the employer could end up facing employer mandate penalty bills. (Image: Allison Bell/ALM)
Big employers that use the new individual coverage health reimbursement arrangement (HRA) programs to replace traditional group health plans for permanent, full-time workers will have to make sure the employees can afford Affordable Care Act exchange plan, according to health care and labor lawyers at Foley Hoag LLP.
The lawyers — Thomas Barker, Christopher Feudo and Ross Margulies — talk about the individual coverage HRA funding issue in an alert analyzing the new individual coverage HRA regulations.
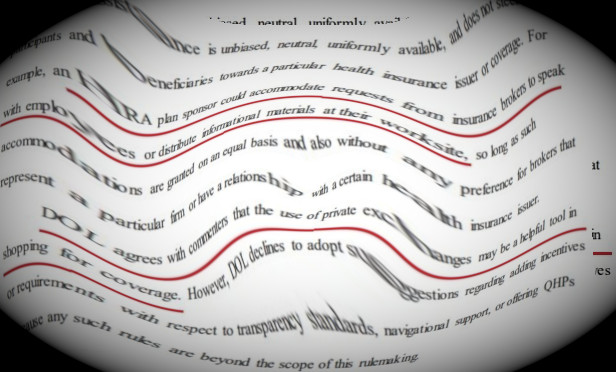
The Internal Revenue Service, the U.S. Department of Labor's Employee Benefits Security Administration, and the U.S. Department of Health and Human Services published the final regulations in June.
Compliance specialists are still finding new wrinkles in the new regulations.
One is that employers big enough to be subject to the ACA “shared responsibility” rules, or employer coverage mandate rules, may have a harder time whether they have successfully avoided having to pay the ACA mandate penalties.
Normally, the lawyers write, an employee who was offered an individual coverage HRA would not be able to use an ACA exchange plan premium tax credit subsidy, and would not be able to lead to the IRS imposing employer coverage mandate penalties.
“If an individual is offered the HRA option, but declines it, the individual may be able to qualify for the credit if the HRA, when combined with individual market coverage, is unaffordable,' the Foley Hoag lawyers write.
If full-time, permanent workers who decline individual coverage HRAs end up qualifying for the ACA exchange plan premium tax credit, the employer could end up facing employer mandate penalty bills.
The Foley Hoag lawyers note that how all of this will really work is unclear.
“The Treasury Department and the IRS are planning to propose new rules on this topic,” the lawyers write.
Another Wrinkle
Edward Fensholt of Lockton Companies wrote in a client alert that another challenge is that individual coverage tends to be more expensive than group coverage.
“In a tight labor market, employers using health insurance as an attraction and retention tool would have to increase HRA contributions, year over year, in amounts that would likely far and away exceed the increases they'd pay for equivalent coverage on a group basis,” Fensholt wrote.
Individual Coverage HRA Basics
An employer could provide an unlimited amount of cash through an individual coverage HRA, as long as the employee used the cash to provide individual coverage or other coverage compatible with Affordable Care Act (ACA) coverage rules.
An employer could also contribute up to $1,800 per year that an employee could use for buying “excepted benefits,” such as dental insurance and hospital indemnity insurance.
Regulation impact analysts at the U.S. Labor Department have estimated the regulations could eventually lead to 800,000 employers replacing their group health plans with individual coverage HRA programs.
The Appeal
William Sweetnam Jr., legislative and technical director at the Employers Council on Flexible Compensation,
He said some employers could see adding an individual coverage HRA program as a good way to top off traditional group health coverage.. “An employer may be concerned that its employees are struggling with deductible and co-pays for the health insurance that they have under the health insurance they have, and they may want to offer a small amount of assistance to them through an HRA,” Sweetnam said.
Read more:
Complete your profile to continue reading and get FREE access to BenefitsPRO, part of your ALM digital membership.
Your access to unlimited BenefitsPRO content isn’t changing.
Once you are an ALM digital member, you’ll receive:
- Breaking benefits news and analysis, on-site and via our newsletters and custom alerts
- Educational webcasts, white papers, and ebooks from industry thought leaders
- Critical converage of the property casualty insurance and financial advisory markets on our other ALM sites, PropertyCasualty360 and ThinkAdvisor
Already have an account? Sign In Now
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.