 Telemedicine and telehealth can improve continuity of care for people with chronic illness by simplifying disease management and making it more accessible and efficient. (Photo: Shutterstock)
Telemedicine and telehealth can improve continuity of care for people with chronic illness by simplifying disease management and making it more accessible and efficient. (Photo: Shutterstock)A growing number of self-insured employers are turning to telemedicine–the provision of health care services through remote consultation, including video chat or other telecommunications–in their quest to improve employee access to high quality health care providers. Often called "remote" or "virtual care," telemedicine has evolved into a powerful, user-friendly means of providing almost immediate access to physicians, while lowering costs by 60 percent to 70 percent compared with traditional brick-and-mortar medicine.
It should come as no surprise then that nearly 60 percent of employers now offer virtual care as a standard benefit for employees, owing to its time and cost effectiveness, and high patient satisfaction. Clinical telemedicine continues to grow and expand beyond its initial intention of treating simple, straightforward acute care complaints. We are now witnessing the emergence of specialty telemedicine and its utilization for chronic disease management (CDM) — the most prevalent and resource-consumptive health conditions.
Related: Corporate culture, chronic disease and the care continuum
Large employers have been the fastest and most notable adopters of telemedicine—from 27 percent in 2015 to 63 percent in 2017, and 82 percent in 2019. Among employers with 50 or more employees that offer telemedicine services, 48 percent use incentives, such as lower cost-sharing — the share of costs covered by insurance that the member pays out of pocket — to encourage its use.
Lower cost-sharing incentives for telemedicine use have been successful in increasing the utilization of telemedicine among employees and lowering overall health costs.
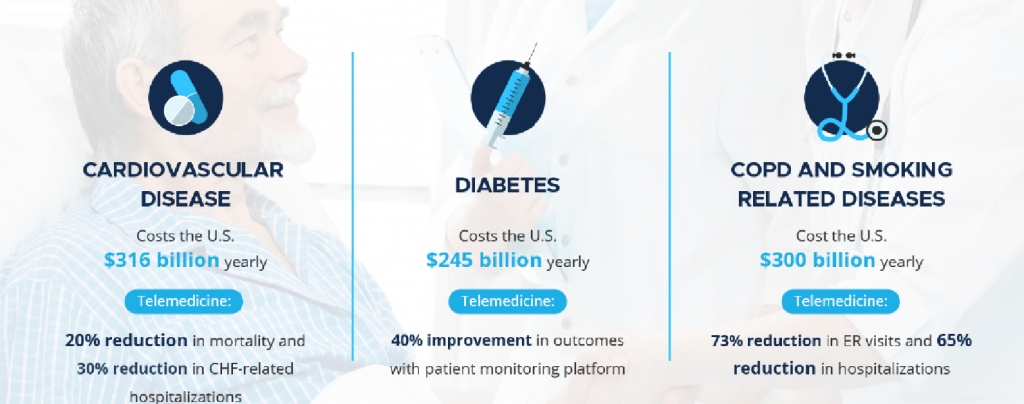
With more employers, brokers, TPAs, payers and their intermediaries touting the importance of embracing telemedicine given its cost savings and time efficiency, specialty telemedicine is expected to become increasingly important for addressing complex, chronic diseases, such as diabetes, heart disease, asthma/COPD and others. Specialty telemedicine provides high quality care, better care coordination and communication, and improved medication/treatment compliance. By addressing clinical issues early in their course, potentially disastrous complications can be avoided, as well as costly visits to the hospital emergency department or urgent care clinic.
Champions of telemedicine believe that this disruptive service can improve the value and efficiency of health care by conveniently monitoring chronic conditions or triaging and managing non-emergency situations. Moreover, this clinical service is location agnostic and can be offered to any patient anywhere, thereby improving access to specialty care in rural communities or areas with limited provider availability.
Simplifying the management of chronic illness
The benefits of telemedicine in CDM are evident and have been demonstrated by multiple studies and reports. Remotely monitoring patients' physiologic and clinical parameters and addressing abnormalities and patient concerns with continuous clinical services, saves money for health care providers, employers, employees and insurance companies.
Telemedicine is particularly beneficial for hourly employees with Minimum Essential Coverage because it allows them to avoid the cost of an expensive ER or urgent care visit.
A growing number of Americans are suffering from more than one chronic condition, putting pressure on health care providers to create care management platforms that address several interconnecting health issues.
Currently, chronic illnesses account for roughly 75 percent of all physician visits, 80 percent of all hospital admissions and 90 percent of all prescriptions. These numbers will only grow as 50 percent of all Americans are projected to suffer some form of chronic illness by 2025, ranging from COPD to HIV. The management of these conditions requires continuity of care, specifically continuous monitoring and feedback, to ensure that the patients can avoid the disease- associated morbidity and mortality, thereby improving, or at least maintaining, the patient's quality of life.
Telemedicine and telehealth can improve continuity of care for people with chronic illness by simplifying disease management and making it more accessible and efficient. Patient's care plans can be streamlined and ordered daily, providing easy access to required care components. Telehealth tools can serve as a source of information and advice for questions that arise. Health information is easily stored and processed, allowing patients to have constant access to their health data. Additionally, care teams can coordinate care for a shared client using a portal with streamlined communication, rather than relying on traditional health records or communication tools, which are often inadequate or incomplete.
Choosing the right telemedicine solution
Look for a partner that includes CDM and a network of medical experts for managing chronic conditions, such as heart disease, chronic lung disease, diabetes and chronic kidney disease. The solution provider should also have broad and diverse experience and, for global companies, a telemedicine service with worldwide capabilities.
Software and platform
Today, leading-edge telemedicine companies rely upon advanced analytics and technology. Some telemedicine companies utilize sophisticated artificial intelligence (AI)-powered software with clinical and telemedicine input to improve outcomes and lower costs for chronically ill patients. Expanded care platforms can address gaps in care in conjunction with other technology, ranging from wireless devices and wearables to mHealth-enabled electronic health care record (EHR) platforms.
CDM telemedicine checklistPersonalized care
Comprehensive care
Collaborative care
|
The patient experience: Using a CDM telemedicine portal
Typically, patients enroll online or by phone, creating an account and completing a short questionnaire regarding medical history, current medical conditions, allergies and medications—similar to the forms required before a doctor's appointment. This information should be securely protected, HIPAA-compliant and shared only with the attending doctor for review before the online consultation.
With some of the more sophisticated telemedicine programs, users can go online either via the computer or app to choose from a list of doctors and specialists, schedule an appointment and arrange an appointment reminder. They can also upload photos and files that might better inform the doctor's diagnosis and care program.
Much like any clinical service, a patient who requires a specialist can be referred either by their primary care physician or via the telemedicine physician who whose diagnosis is based on medical history and current symptoms.
With management of chronic illnesses becoming a focal point of overall case management, it's important to look for a telemedicine platform that provides clinical tools for medical conditions including chronic illnesses. Such tools could include daily care plans, the ability to track and log activities and food intake—much like any popular health tracker app—and provide medical alerts to help patients remain compliant with their medication and treatment regimen.
A person with diabetes, for example, should receive a checklist for maintaining optimal health based on their condition and pre-set parameters including reminders to check their sugar level and take insulin. Severe deviations from the patient's baseline levels should trigger an alert to the care team.
The best CDM telemedicine solutions rely on AI engines that can learn the patient's tolerances, habits and variances based on their input, and run detailed reports and trends that provide a larger picture of the patient's progress.
The age of "new medicine"
Telemedicine and telehealth provide a breed of "new medicine" and represent a vast improvement over traditional medicine in the days when patients, particularly those with chronic medical conditions, would have to constantly visit the doctor's office or access emergency help. The great innovation of telemedicine is that medical care is decentralized and democratized, easily accessible and of the highest quality.
As a 21st century way for physicians to take care of patients—and patients to manage their chronic illnesses–CDM telemedicine harnesses technology to better engage the patient, improve outcomes and, concurrently, enable self-insured employers to provide cost-effective quality care for individuals with chronic conditions.
Dr. Jonathan Wiesen, M.D., is founder and Chief Medical Officer at MediOrbis.
Read more:
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to asset-and-logo-licensing@alm.com. For more information visit Asset & Logo Licensing.







