 For the 10 percent scenario, the study estimated total costs in the $56 billion to $93 billion range, for the 2020-2021 time period. (Photo: Shutterstock)
For the 10 percent scenario, the study estimated total costs in the $56 billion to $93 billion range, for the 2020-2021 time period. (Photo: Shutterstock)
The health care costs of the COVID-19 pandemic in the US is just beginning to come into focus, with a range of estimates on what those costs could be. The latest, from the nation's largest health insurance industry group, predicts costs between $56 billion to $556 billion over the next two years—depending on many factors, including how many Americans are infected, how widely social distancing efforts are adopted, and the availability of testing and other medical resources.
The new analysis was released by America's Health Insurance Plans (AHIP), based on research by Wakely, an actuarial group that specializes in health care. AHIP notes that the research is based on data available as of March 28, and with the rapidly changing realities of a worldwide pandemic, will need to be revised over time.
"Protecting Americans' health and financial stability always has been, and always will be, our first priority," said Matt Eyles, president and CEO of AHIP in a statement released with the report. "This new data provides us with better insight to help policymakers, private sector leaders, and other stakeholders understand the investments required to successfully care for every American subjected to this life-threatening virus."
Three possible scenarios for costs
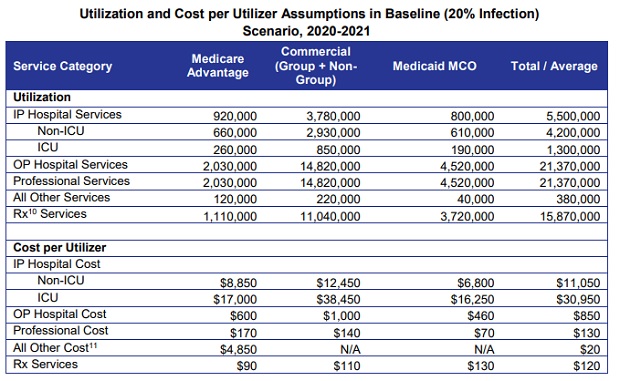
The Wakely researchers acknowledged that the result of the COVID-19 pandemic could result in an "astonishingly broad range of potential outcomes." With that caveat, the report breaks down costs into three possible scenarios, based on possible rates of infection, set at 10 percent, 20 percent, and 60 percent of the US population. These cost estimates include inpatient hospital costs, outpatient costs, costs for professional and other services, and prescription drug costs.
 (Source: AHIP)
(Source: AHIP)- For the 10 percent scenario, the study estimated total costs in the $56 billion to $93 billion range, for the 2020-2021 time period.
- With a 20 percent infected rate for the population, the report estimated total costs in the $113 billion to $185 billion range for the same two-year period.
- For the "high infection rate" scenario, at 60 percent of the population, the total cost range is $337 billion to $556 billion.
The report also noted that it is possible a vaccine will be approved and distributed during this two-year time span. "While the costs of the vaccine are unknown, [they] could be significant," the report said. "For example, if a cost per inoculation is $500 and the majority (80 percent) of the population gets vaccinated in 2021, this alone would add over $100 billion to the total cost estimate."
Enrollee cost-sharing estimates
The Wakely study also looked at how the insurance industry would share these costs with enrollees. The researchers assumed zero cost-sharing for Medicaid plan enrollees, since recent funding bills from Congress call for federal payments to providers to cover those costs. The report said the enrollee cost-sharing outside of Medicaid is likely to be around 14 percent to 18 percent of annual allowed costs. For the three scenarios, that breaks down to: $10 billion to $13 billion of cost-sharing by enrollees for the 10 percent infection rate, $20 billion to $26 billion for the 20 percent rate, and $60 billion to $78 billion for the 60 percent infection rate.
AHIP noted in its statement that this cost-sharing figure does not take into account the fact that a number of health insurance carriers have said that they will waive out-of-pocket costs for COVID 19 and treatment.
"Costs should not be a barrier to anyone seeking treatment," said Eyles. "This is why many health insurance providers have stepped forward to proactively waive out-of-pocket costs for testing and treatment. These essential actions are ensuring that both the health and financial stability of hundreds of millions of Americans are protected at a time they need it most. And for hospitals, it eliminates the need to bill and collect from patients so they can focus on caring for their patients."
Read more:
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.







