Telemedicine offerings as part of comprehensive health care plans grew over the last decade, as advisors worked with employers to keep health care costs down while meeting the varied and changing needs of employees. However, by 2018, only 2% of the employee population covered by telemedicine actually utilized the service. The widespread underuse of telemed offerings seemed like wasted health care dollars that could have been better utilized elsewhere.
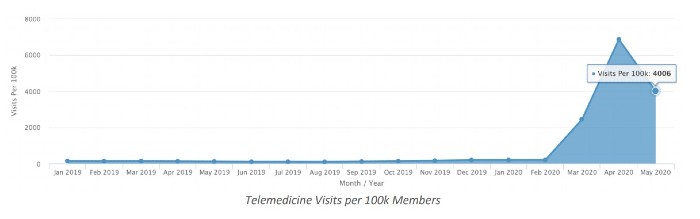
The explosion of COVID-19 in the United States has changed the health care landscape as we know it — and telemedicine is no exception. There has been an unprecedented rise in telemedicine utilization throughout 2020. Innovu tracked a 2,100% increase in telemed use through May of 2020. While that number dipped recently as in-person visits rose over the summer, due to ongoing waves of COVID-19 and flu, advisors and employers should continue to encourage employees to use telemedicine services whenever possible.
Why telemedicine matters
With a lower cost per visit than traditional office visits and more comfort and safety for patients and providers alike, using telemedicine for common colds, ailments, dermatology, and therapy, can save employers and employees time and money.
Recommended For You
Complete your profile to continue reading and get FREE access to BenefitsPRO, part of your ALM digital membership.
Your access to unlimited BenefitsPRO content isn’t changing.
Once you are an ALM digital member, you’ll receive:
- Breaking benefits news and analysis, on-site and via our newsletters and custom alerts
- Educational webcasts, white papers, and ebooks from industry thought leaders
- Critical converage of the property casualty insurance and financial advisory markets on our other ALM sites, PropertyCasualty360 and ThinkAdvisor
Already have an account? Sign In Now
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.









