Credit: New Africa/Adobe Stock
Credit: New Africa/Adobe Stock
Over 40% of people in the U.S. are living with obesity and over 11% have Type 2 Diabetes. Metabolic disease is a public health crisis that is driving unsustainable health care spending. Diabetes care alone now exceeds $410 billion annually, with much of that burden shouldered by employers, who cover direct costs like medication and treatment, and individuals who face expensive co-pays and rising health insurance premiums.
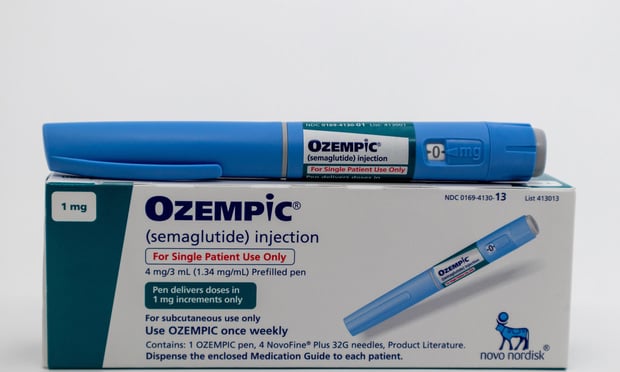
GLP-1s have introduced both opportunity and complexity to this already convoluted landscape. While many health plans and employers are still reeling from sticker shock, the potential of this promising new class of drugs to combat obesity by inducing weight loss is undeniable.
Recommended For You
While this class of drugs is not for everyone, our understanding of their appropriateness and optimal use is continuing to evolve. Much of this, researchers are beginning to understand, can be determined by an individual’s metabolism.
GLP-1s will certainly help many kickstart their weight loss journey. But without personalized programs that address the root causes of metabolic dysfunction, such as insulin resistance and inflammation, employers can expect as much as a quarter of their GLP-1 spending to continue going to waste.
Understanding responder types
Approximately 2 out of 3 people stop taking GLP-1s within 12 months due to unwanted side effects, out-of-pocket costs, the desire to avoid long-term reliance on injections, or perhaps most commonly, because they don’t experience sustained weight loss.
For most, GLP-1s trigger a strong initial response. Maintaining weight loss beyond this initial phase is not guaranteed. Human metabolism is incredibly complex and unique to each individual. Each individual’s metabolic response to GLP-1s, in turn, varies – but they will generally fall into one of three buckets:
- Super responders: People who lose at least 10% of their body weight at any point during their treatment.
- General responders: People who lose at least 5% of their body weight within three months.
- Non-responders: People who lose less than 5% of their body weight after three months of treatment.
While GLP-1s can help individuals start on a path to weight loss, they aren’t designed to provide lasting metabolic health alone. People need an exit strategy to sustain weight loss without high-cost medications. To realize the best health outcomes and optimize GLP-1 spending, employers should follow these five guiding principles.
5 principles for optimizing GLP-1 spend
- Preserve and enable choice. Everyone should have the opportunity to exercise choice in their health care journey. Regular injections are not for everyone, but for many, GLP-1s are an optimal initial choice. Those individuals deserve the right to access the drug if they meet clinical criteria.
- Maximize GLP-1 benefits with personalized algorithms and nutrition plans. Key to optimizing GLP-1 spend is an individual’s ability to understand their metabolism on a deep level. The metabolism is like a black box; without real-time insight into key metabolic health factors like blood glucose, sleep, stress, and activity, creating a sustainable treatment plan for metabolic disease is little more than taking a guess. Employers should be able to arm their employees with these insights, and their solutions should be able to use them to develop personalized plans to help individuals maximize and sustain the benefits of GLP-1s.
- Understand every person’s GLP-1 responder class. Whether they’re super responders, general responders, or non-responders, the impact of GLP-1s will vary for every individual. It’s essential to monitor and understand when it’s working on an individual level and ensure combining lifestyle modification to optimize weight loss impact regardless of GLP-1 response phenotype.
- Adjust GLP-1 treatment accordingly. Likewise, it is critical to have insight into how members respond to GLP-1s based on their unique metabolic composition. For every employer, being able to monitor when the drug stops being effective for their employees will be the difference between optimization and waste.
- Effectively reduce the dose over time. For most, GLP-1s are not sustainable for life. It’s important to provide individuals with precise, long-term interventions that extend beyond the maximum benefit window of GLP-1s. Plans and employers should have an off-ramp strategy to help individuals sustain weight loss in the weeks, months, and years after eliminating GLP-1s.
Dr. Lisa Shah is an internist and the chief medical officer of Twin Health, a health AI company using digital twin technology to reverse and prevent metabolic diseases.
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.