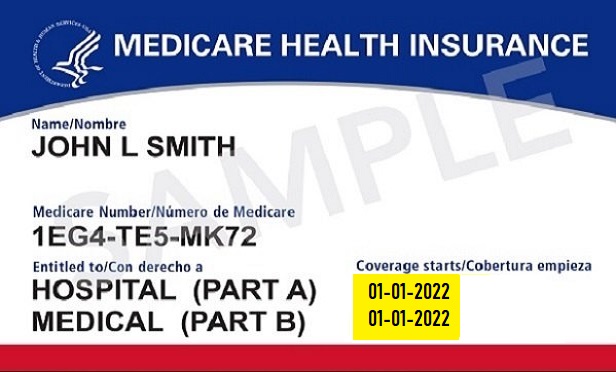
 A Medicare card
A Medicare card
Medicare is undergoing significant changes this year, including a long-awaited $2,000 cap on annual out-of-pocket prescription drug costs, expanded telehealth access and efforts to improve provider networks.
While these updates aim to enhance affordability and accessibility, many beneficiaries are facing unexpected hurdles.
Recommended For You
Insurers are modifying drug formularies, Medicare Advantage provider directories can be misleading, and new telehealth restrictions are limiting virtual care options.
These challenges raise an important question: If Medicare is expanding benefits, why are some of your employees who have Medicare coverage struggling to access care?
One medicare beneficiary's perspective
A Medicare enrollee recently asked, "If Medicare is expanding benefits, why can't I access care?"
"I was relieved to hear about the $2,000 drug cap and expanded telehealth access, but I'm still struggling to get the care I need," the enrollee said.
"Some of my medications are no longer covered, my doctor says they don't accept my plan, and my telehealth visits keep getting denied.
If Medicare is expanding benefits, why is it getting harder to use them?"
While the Centers for Medicare and Medicaid Services has introduced policies to enhance affordability and accessibility, insurers and providers are making behind-the-scenes adjustments that may limit patient access.
Hidden impact of Medicare Part D out-of-pocket cap
One of the most widely publicized Medicare changes for this year is the $2,000 cap on annual out-of-pocket prescription drug costs—a provision of the Inflation Reduction Act of 2022.
This reform is expected to lower costs for seniors taking expensive medications for conditions such as cancer, multiple sclerosis and diabetes.
However, some industry analysts insurers are adjusting their Part D formularies in response to the cap.
How insurers may respond:
Restricting coverage for high-cost medications:
◆ Insurers may move expensive drugs to higher formulary tiers, requiring higher cost-sharing and stricter prior authorization rules.
◆ Some medications could be removed from formularies, forcing patients to switch treatments.
Potential reductions in manufacturer assistance programs:
◆ Previously, once enrollees reached catastrophic coverage, drug manufacturers often provided financial assistance.
◆ With the new $2,000 cap, some pharmaceutical companies have signaled potential reductions in assistance programs, though details remain unclear.
Challenges with the "smoothing feature":
◆ CMS introduced a new cost "smoothing" option, allowing enrollees to spread their drug costs over the year instead of paying large amounts at once.
◆ However, some pharmacies and insurers may not be fully prepared to implement this system, leading to confusion.
What your employees can do
In light of these changes, Medicare participants can:
◆ Review formulary changes during Medicare open enrollment.
◆ Work with their healthcare providers to appeal denied drug coverage.
◆ Confirm with pharmacies whether the smoothing program is available before relying on it.
Medicare ghost network problem
For years, Medicare Advantage enrollees have struggled with provider directories listing doctors who do not actually accept the plan—a "ghost network" issue.
Despite CMS rules requiring Medicare Advantage insurers to update directories every 90 days, a 2023 Office of Inspector General (OIG) report found persistent inaccuracies.
Some provider directory errors remained unresolved for more than a year, leaving seniors struggling to find an in-network doctor.
Many physicians listed as available were retired, not taking new patients, or no longer accepting Medicare Advantage plans.
The reasons ghost networks persist include:
◆ High provider turnover can make directories difficult to maintain.
◆ Some insurers may list extra providers to make their networks appear larger.
◆ CMS enforcement is inconsistent, with minimal penalties for inaccurate directories.
The potential impact on beneficiaries includes:
Delays in care: Seniors may spend weeks or months searching for an actual in-network provider.
Unexpected out-of-pocket costs: Some beneficiaries unknowingly visit out-of-network providers and receive surprise medical bills.
Frustration and confusion: Patients must call multiple offices before finding a doctor who accepts their plan.
Related: UnitedHealth wins ruling over $2B in alleged Medicare Advantage overpayments
What your clients can do
◆ Call doctors' offices directly to confirm network participation before enrolling.
◆ Use Medicare's Physician Compare tool on Medicare.gov to verify provider information.
◆ Report inaccurate directories to CMS at 800-MEDICARE to push for better enforcement.
Why virtual care is harder to access
During the COVID-19 pandemic, Medicare expanded telehealth coverage, allowing beneficiaries to access doctors nationwide.
Many assumed these flexibilities would continue indefinitely.
However, some pandemic-era telehealth policies will expire this year, leading to concerns about reduced access.
Despite Medicare's efforts to expand benefits and improve affordability, many seniors continue to face significant barriers to care.
Insurers adjusting drug formularies, inaccurate provider directories, and new telehealth restrictions are creating unintended challenges that undermine the intended impact of these reforms.
While CMS policies aim to enhance access, enforcement gaps and industry responses often leave beneficiaries navigating a complex system on their own.
As policymakers evaluate these ongoing challenges, seniors must stay proactive.
Checking provider participation, reviewing drug formularies during open enrollment, and advocating for stronger oversight will be essential to ensuring that Medicare's evolving benefits translate into real-world access.
Tricia Blazier, JD, is director of Healthcare Insurance Services at Allsup.
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.








