UMR
Company Info

TOPIC IN FOCUS
The latest news and developments that advisors need to create meaningful tax planning strategies for clients.
MORE TO EXPLORE
Expert Perspectives is the home to the voices of industry leaders, as they share their expertise and insights directly from the field.
Discover relevant content from across the suite of ALM legal publications
Media & Resources
With health care spending rising, payment integrity solutions can play an increasingly important role in how brokers help clients reduce costs.
Advocacy service models use data and tech innovation to help streamline information, increase quality of health care and save money.
Hospitals are reexamining their health plans to address medical cost trend and add options that stand out in a highly competitive labor market.


From Optavise
Download this white paper to explore how voluntary benefits serve as crucial risk management tools for employers, mitigating the financial burden of workers’ compensation.
Download Resource
From Zelis
The accuracy of your provider directories is vital to shaping your success. The guide provides actionable insights and best practices for ensuring the data you rely on is precise and trustworthy.
Download Resource
From Labcorp
High blood pressure affects nearly half of U.S. adults, increasing the risk of heart disease and stroke. This case study explores how an employer-sponsored wellness program helped approximately 1 in 3 employees improve their blood pressure risk level.
Download Resource
From Labcorp
Long onboarding times and staffing shortages create costly delays. Discover how one large healthcare system streamlined its hiring process, reducing onboarding time from weeks to days while improving the candidate experience and freeing up internal staff.
Download Resource
From Trustmark Voluntary Benefits
Voluntary benefit elections are not what they used to be. The shift toward passive enrollments prevents employees from being actively engaged in the enrollment process, generating low participation rates and putting employers and insurers at risk. This guide explores a new approach to enrollment that combines facets of both traditional enrollment processes and the new self-service culture to increase engagement and boost participation.
Download Resource
From ArmadaCare
Get a handle on supplemental health insurance--fast. This quick-reference guide breaks down voluntary vs. employer-paid plans, coverage types, and when to recommend each. Ideal for brokers advising clients on modern benefits strategies.
Download Resource
From Noom Health
Your workforce's well-being is shaped by more than just what happens on the job. Environmental factors, such as housing stability and food security, can significantly impact your employee’s performance at work. This playbook equips HR leaders with the knowledge and insights they need to design equitable, inclusive benefits programs that address real-world problems to boost employee health and improve your bottom line.
Download Resource
From Nationwide® pet insurance
Today’s employees expect more than just health insurance. Learn how pet insurance is becoming a must-have voluntary benefit--especially for millennials and Gen Z. This infographic gives benefits brokers the data and insights needed to stay ahead in a competitive labor market.
Download Resource
From Noom Health
An employee’s well-being and performance are influenced by external factors, such as the communities they live in and access to affordable, nutritious food. This playbook equips benefits brokers with the knowledge and strategies they need to support clients in addressing these and other environmental factors to create an equitable, inclusive benefits program that addresses real-world challenges and boosts employee performance.
Download Resource
From Nationwide® pet insurance
Millennials and Gen-Z are now the leading workforce generations, and employers are faced with the challenge of adapting to the new set of values they bring with them. These younger employees expect flexibility and benefits that support all aspects of their lives, including their pets. Discover how pet insurance can help strengthen client retention, meet expectations, and support recruitment goals.
Download Resource
From Zelis
Inaccurate provider data can lead to frustrated clients and stress on your business relationships. These are the top do’s and don’ts to ensure the data you rely on as a benefits advisor is as accurate and helpful as possible.
Download Resource
From LifeSecure Insurance Company
Employers are revamping their benefits strategies--but are they offering what employees truly want? Discover the seven key elements shaping workplace benefits in 2025 to help your clients enhance satisfaction, retention, and enrollment.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
In 2025, you are uniquely positioned to make a real difference for your clients--both financially and in the wellness of their employees. Full of tips ranging from goal setting to relationship building, this is your guide to being a better partner this year, and beyond.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
Explore alternative plan designs, including HSAs, HRAs, QSEHRAs, ICHRAs, and MERPs, in this brief e-book.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
Discover innovative solutions to help your clients overcome cost barriers in health insurance.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
Prioritizing health equity can transform your sales strategy and secure long-term business success. This guide helps you lead thoughtful conversations by aligning with employers' values.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
You can bet that many of your employer clients will be considering alternative funding models as they shop around for health plans this year. Download this short guide to learn about the difference between MERPs and HRAs, why they matter and how you can provide your clients with lower costs, more flexibility and greater satisfaction.
Download Resource
From Zelis
Managing health plan data is complex and time-consuming. Brokers need seamless access to accurate, up-to-date provider and network information to effectively guide employers and beneficiaries. This resource explores how to streamline workflows, reduce manual data handling, and enhance decision-making with smarter solutions.
Download Resource
From ArmadaCare
Are HDHPs & HSAs really the best solution? Let’s take a closer look.
Download Resource
From Nova Healthcare Administrators, Inc.
Healthcare costs are rising, and self-funded employers need a smarter approach. Discover how medical management can enhance cost efficiency and care quality. Download now to explore proven strategies and real-world success stories.
Download Resource
From Nova Healthcare Administrators, Inc.
Open enrollment is your chance to shine as a strategic partner. This guide equips benefit advisors with 5 actionable tips to help clients reduce confusion, streamline processes, and deliver exceptional value to their employees.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
Four industries, one health plan that delivers real savings and better benefits. See how a nonprofit, a wholesale distributor, a health center, and a school district reduced costs and eliminated copays and deductibles--without taking on additional risk. Download the case study bundle to explore how first-dollar coverage can make a difference for your clients.
Download Resource
From ArmadaCare
Help your clients make informed decisions about executive medical reimbursement plans while ensuring compliance amidst evolving regulations.
Download Resource
From New Benefits
Explore four strategies that benefits advisors can leverage to help their clients reduce healthcare expenses.
Download Resource
From Nova Healthcare Administrators, Inc.
Guiding your clients to the right network solution is vital for balancing costs, access, and employee satisfaction. Use this eBook as a strategic and educational tool to provide clarity for your clients around the ins and outs of network solutions.
Download Resource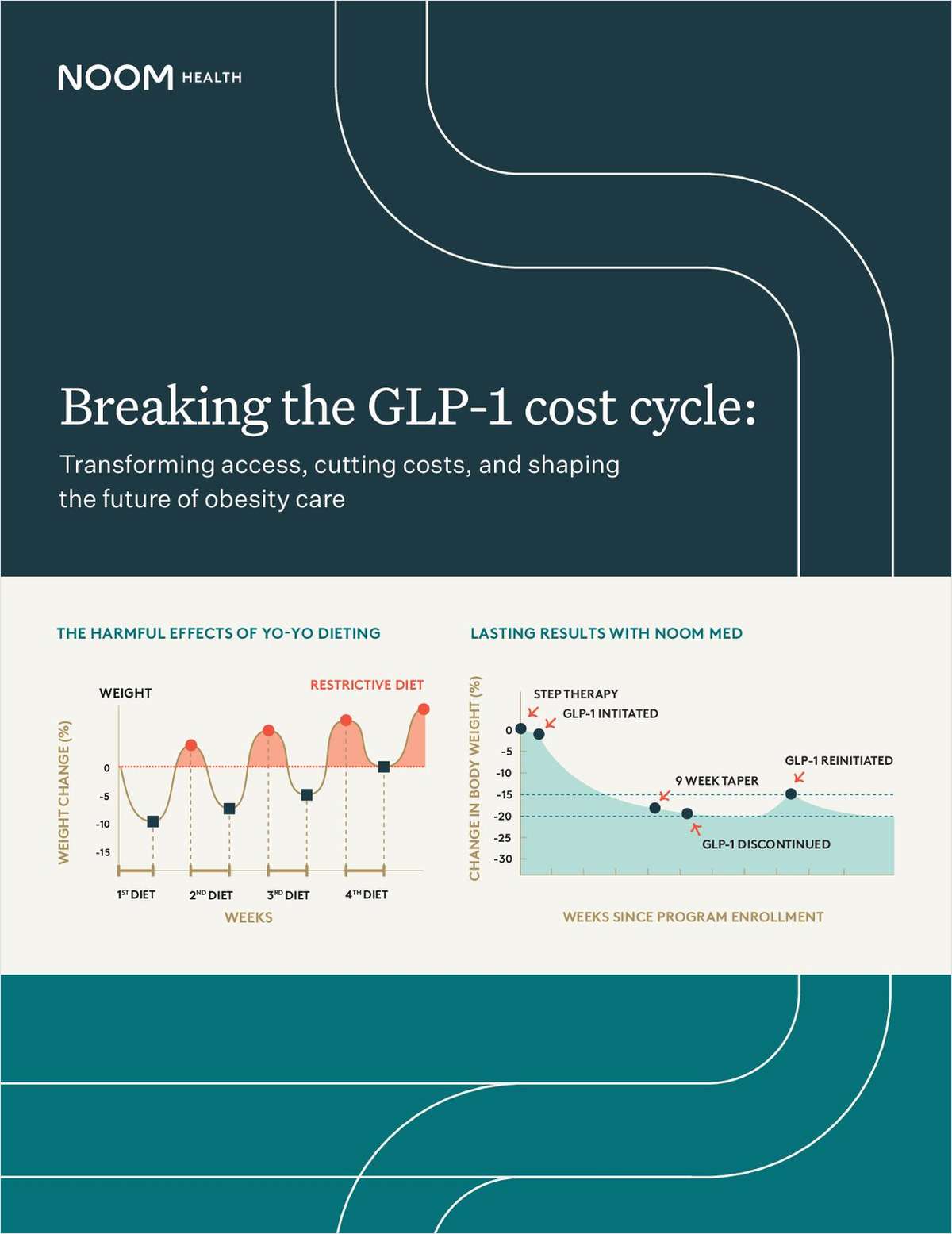
From Noom Health
As obesity rates rise, GLP-1 medications are gaining popularity. Yet, the multifactorial obesity epidemic presents challenges for your clients as more of their employees demand GLP-1’s. This white paper explores strategies to help clients cut costs, improve employee health outcomes, and achieve a measurable ROI.
Download Resource
From New Benefits
This report reveals the top non-insured benefits that not only reduce costs but also address the rising challenges of burnout, financial stress, and work-life balance. Give your clients the edge they need to support their employees while driving business growth. Download the report now to learn more!
Download Resource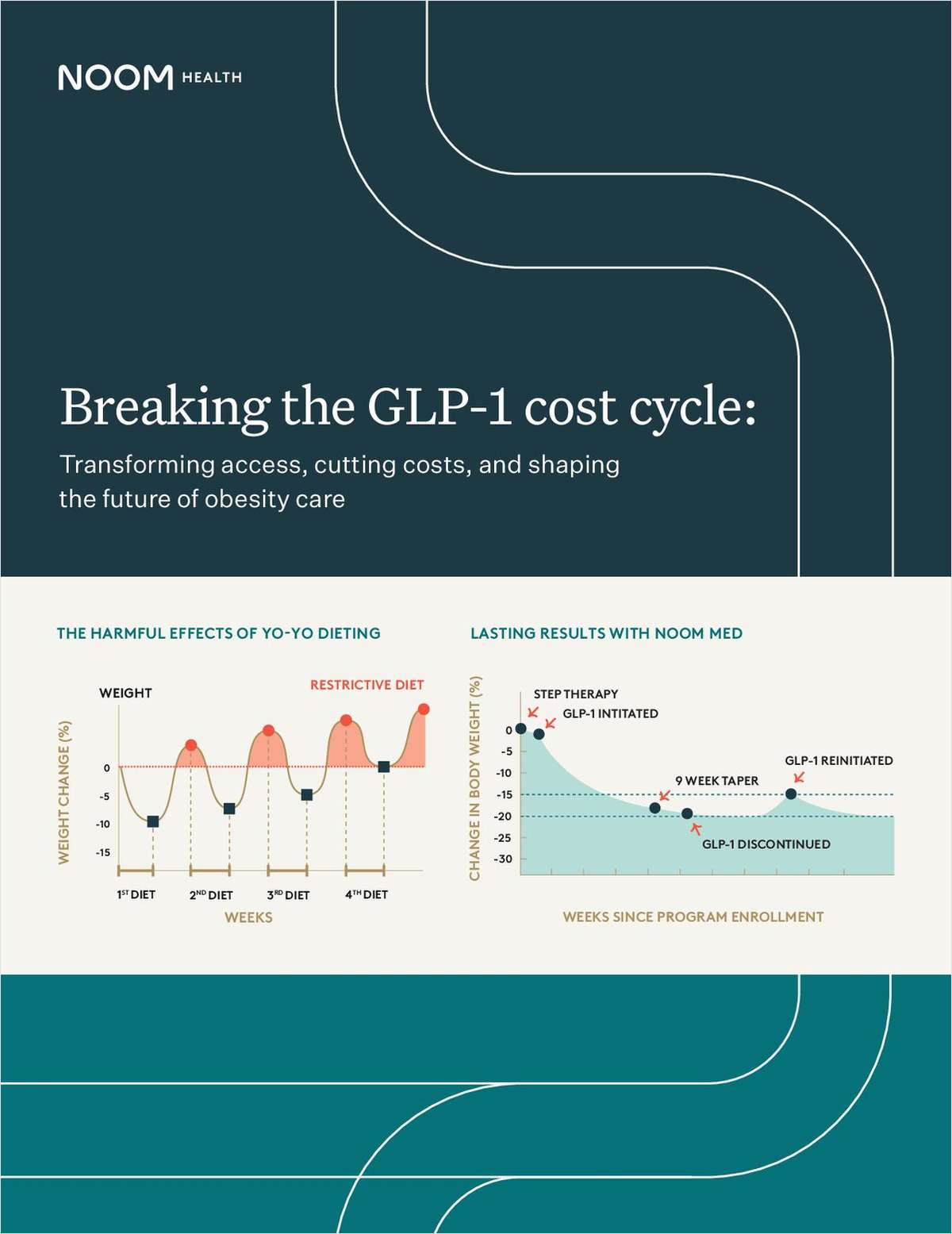
From Noom Health
As obesity rates rise, GLP-1 medications are gaining popularity. Yet, the multifactorial obesity epidemic presents challenges for organizations as more employees seek GLP-1’s. This white paper explores actionable strategies to help cut costs, improve employee health outcomes, and achieve a measurable ROI.
Download Resource
From ArmadaCare
Are brokers prepared for what’s next? See the 5 hot benefits trends shaping 2025 in this report.
Download Resource
From Optavise
Download this white paper to explore how voluntary benefits serve as crucial risk management tools for employers, mitigating the financial burden of workers’ compensation.
Download Resource
From Zelis
The accuracy of your provider directories is vital to shaping your success. The guide provides actionable insights and best practices for ensuring the data you rely on is precise and trustworthy.
Download Resource
From Labcorp
High blood pressure affects nearly half of U.S. adults, increasing the risk of heart disease and stroke. This case study explores how an employer-sponsored wellness program helped approximately 1 in 3 employees improve their blood pressure risk level.
Download Resource
From Labcorp
Long onboarding times and staffing shortages create costly delays. Discover how one large healthcare system streamlined its hiring process, reducing onboarding time from weeks to days while improving the candidate experience and freeing up internal staff.
Download Resource
From Trustmark Voluntary Benefits
Voluntary benefit elections are not what they used to be. The shift toward passive enrollments prevents employees from being actively engaged in the enrollment process, generating low participation rates and putting employers and insurers at risk. This guide explores a new approach to enrollment that combines facets of both traditional enrollment processes and the new self-service culture to increase engagement and boost participation.
Download Resource
From ArmadaCare
Get a handle on supplemental health insurance--fast. This quick-reference guide breaks down voluntary vs. employer-paid plans, coverage types, and when to recommend each. Ideal for brokers advising clients on modern benefits strategies.
Download Resource
From Noom Health
Your workforce's well-being is shaped by more than just what happens on the job. Environmental factors, such as housing stability and food security, can significantly impact your employee’s performance at work. This playbook equips HR leaders with the knowledge and insights they need to design equitable, inclusive benefits programs that address real-world problems to boost employee health and improve your bottom line.
Download Resource
From Nationwide® pet insurance
Today’s employees expect more than just health insurance. Learn how pet insurance is becoming a must-have voluntary benefit--especially for millennials and Gen Z. This infographic gives benefits brokers the data and insights needed to stay ahead in a competitive labor market.
Download Resource
From Noom Health
An employee’s well-being and performance are influenced by external factors, such as the communities they live in and access to affordable, nutritious food. This playbook equips benefits brokers with the knowledge and strategies they need to support clients in addressing these and other environmental factors to create an equitable, inclusive benefits program that addresses real-world challenges and boosts employee performance.
Download Resource
From Nationwide® pet insurance
Millennials and Gen-Z are now the leading workforce generations, and employers are faced with the challenge of adapting to the new set of values they bring with them. These younger employees expect flexibility and benefits that support all aspects of their lives, including their pets. Discover how pet insurance can help strengthen client retention, meet expectations, and support recruitment goals.
Download Resource
From Zelis
Inaccurate provider data can lead to frustrated clients and stress on your business relationships. These are the top do’s and don’ts to ensure the data you rely on as a benefits advisor is as accurate and helpful as possible.
Download Resource
From LifeSecure Insurance Company
Employers are revamping their benefits strategies--but are they offering what employees truly want? Discover the seven key elements shaping workplace benefits in 2025 to help your clients enhance satisfaction, retention, and enrollment.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
In 2025, you are uniquely positioned to make a real difference for your clients--both financially and in the wellness of their employees. Full of tips ranging from goal setting to relationship building, this is your guide to being a better partner this year, and beyond.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
Explore alternative plan designs, including HSAs, HRAs, QSEHRAs, ICHRAs, and MERPs, in this brief e-book.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
Discover innovative solutions to help your clients overcome cost barriers in health insurance.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
Prioritizing health equity can transform your sales strategy and secure long-term business success. This guide helps you lead thoughtful conversations by aligning with employers' values.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
You can bet that many of your employer clients will be considering alternative funding models as they shop around for health plans this year. Download this short guide to learn about the difference between MERPs and HRAs, why they matter and how you can provide your clients with lower costs, more flexibility and greater satisfaction.
Download Resource
From Zelis
Managing health plan data is complex and time-consuming. Brokers need seamless access to accurate, up-to-date provider and network information to effectively guide employers and beneficiaries. This resource explores how to streamline workflows, reduce manual data handling, and enhance decision-making with smarter solutions.
Download Resource
From ArmadaCare
Are HDHPs & HSAs really the best solution? Let’s take a closer look.
Download Resource
From Nova Healthcare Administrators, Inc.
Healthcare costs are rising, and self-funded employers need a smarter approach. Discover how medical management can enhance cost efficiency and care quality. Download now to explore proven strategies and real-world success stories.
Download Resource
From Nova Healthcare Administrators, Inc.
Open enrollment is your chance to shine as a strategic partner. This guide equips benefit advisors with 5 actionable tips to help clients reduce confusion, streamline processes, and deliver exceptional value to their employees.
Download Resource
From Nonstop Administration and Insurance Services, Inc.
Four industries, one health plan that delivers real savings and better benefits. See how a nonprofit, a wholesale distributor, a health center, and a school district reduced costs and eliminated copays and deductibles--without taking on additional risk. Download the case study bundle to explore how first-dollar coverage can make a difference for your clients.
Download Resource
From ArmadaCare
Help your clients make informed decisions about executive medical reimbursement plans while ensuring compliance amidst evolving regulations.
Download Resource
From New Benefits
Explore four strategies that benefits advisors can leverage to help their clients reduce healthcare expenses.
Download Resource
From Nova Healthcare Administrators, Inc.
Guiding your clients to the right network solution is vital for balancing costs, access, and employee satisfaction. Use this eBook as a strategic and educational tool to provide clarity for your clients around the ins and outs of network solutions.
Download Resource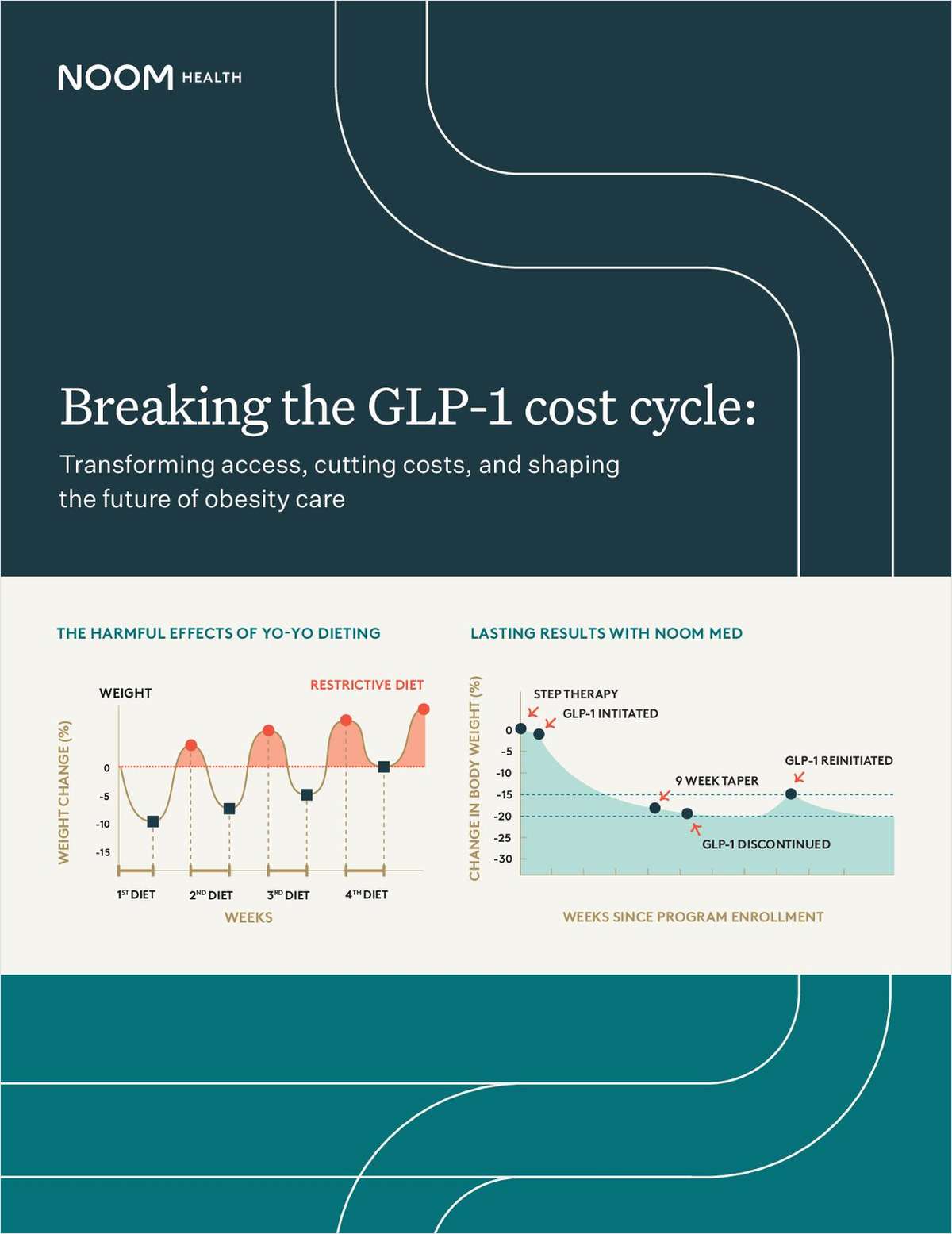
From Noom Health
As obesity rates rise, GLP-1 medications are gaining popularity. Yet, the multifactorial obesity epidemic presents challenges for your clients as more of their employees demand GLP-1’s. This white paper explores strategies to help clients cut costs, improve employee health outcomes, and achieve a measurable ROI.
Download Resource
From New Benefits
This report reveals the top non-insured benefits that not only reduce costs but also address the rising challenges of burnout, financial stress, and work-life balance. Give your clients the edge they need to support their employees while driving business growth. Download the report now to learn more!
Download Resource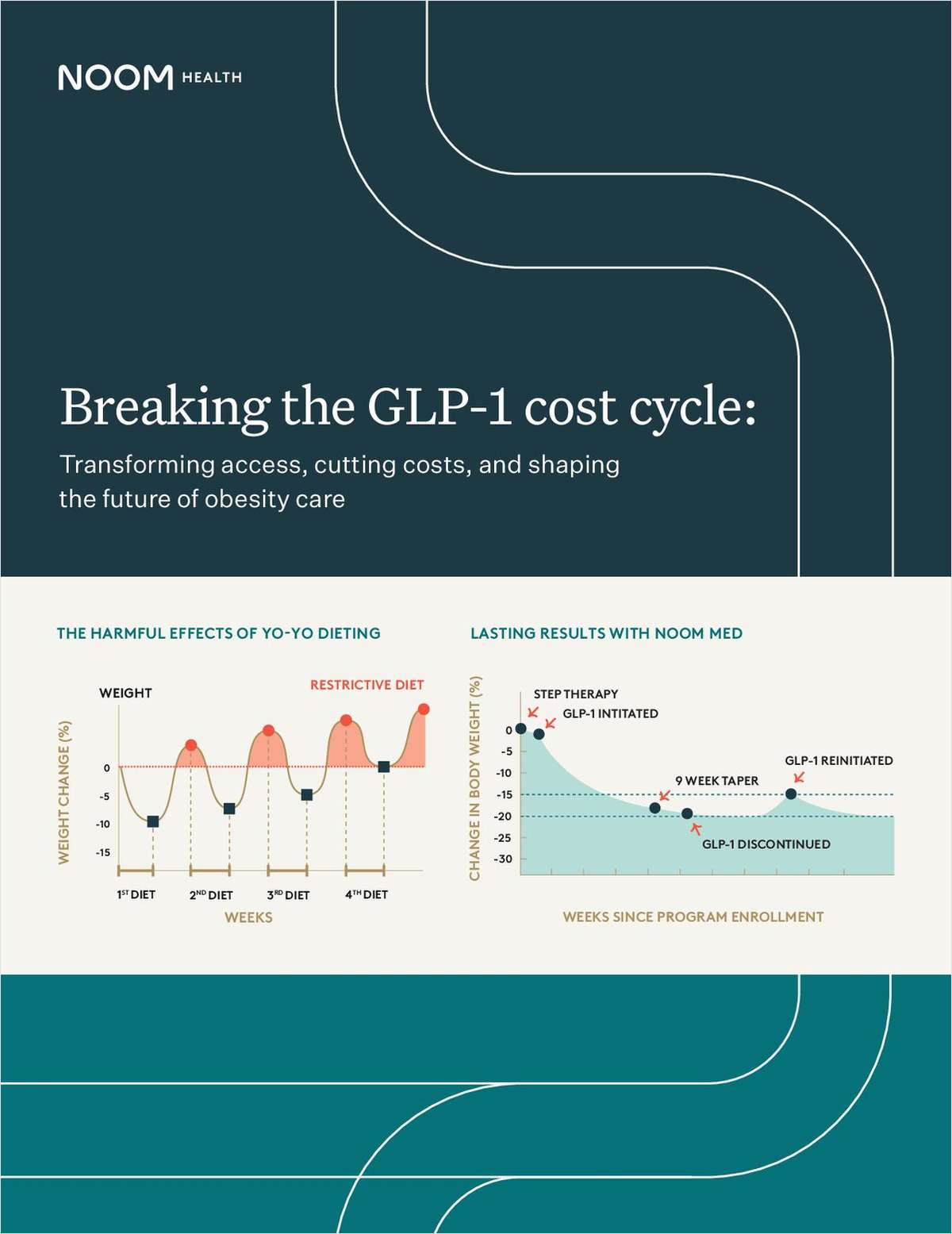
From Noom Health
As obesity rates rise, GLP-1 medications are gaining popularity. Yet, the multifactorial obesity epidemic presents challenges for organizations as more employees seek GLP-1’s. This white paper explores actionable strategies to help cut costs, improve employee health outcomes, and achieve a measurable ROI.
Download Resource
From ArmadaCare
Are brokers prepared for what’s next? See the 5 hot benefits trends shaping 2025 in this report.
Download Resource
From Optavise
Download this white paper to explore how voluntary benefits serve as crucial risk management tools for employers, mitigating the financial burden of workers’ compensation.
Download Resource


