 Credit: K KStock/Adobe stock
Credit: K KStock/Adobe stock
The popularity of weight-loss drugs are growing and local governments say their health care budgets can't keep up.
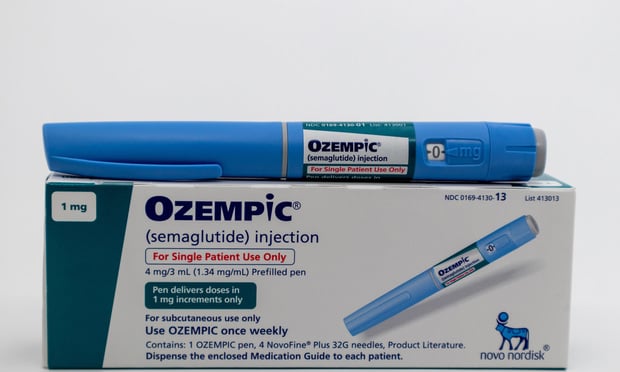
GLP-1s, such as Ozempic and Mounjaro, are a class of drugs that were initially developed to treat type 2 diabetes — which is the most expensive chronic condition in the US, according to Bloomberg. But now, more and more Americans are relying on them for weight loss.
Recommended For You
With the price of GLP-1s reaching well over $1000 a month, local officials are warning that rising costs threaten to quickly drain government spending accounts.
The demand for these drugs isn't slowing down. Bloomberg found that "more than 1 in 10 Americans have type 2 diabetes, and an upward of 100 million suffer from obesity." These rates are even higher among the 19% of Americans who rely on Medicaid.
According to Bloomberg, data shows that diabetes, not obesity, is likely responsible for the surge in spending on GLP-1s. Bloomberg found that new drug formulations, health benefits beyond diabetes and the probability that the drugs will soon be available in pill form is likely to encourage even more patients to take GLP-1s in coming months.
In 2020, reimbursements for GLP-s drugs cost Medicaid $3.3 billion, a rate that skyrocketed to $7.9 billion in 2022. Now, state leaders say they might have to implement new regulations on the drugs in order to control high costs.
In July, Connecticut initiated new hurdles for state employees who were seeking treatment for weight-loss after spending on GLP-1s rose 50% annually since 2020. Later in June, Virginia imposed similar restrictions for Medicaid enrollees. Other states have warned of similar restraints.
Fears are rising about how officials will ration access to GLP-1s and who gets them versus who doesn't. In North Carolina, a state-health board voted that existing members of the plan would remain covered, but all new patients would have to pay out of pocket for the drugs.
Some medical officials now worry that patients will miss out on life-saving treatments due to the excessively high cost of GLP-1s.
© 2025 ALM Global, LLC, All Rights Reserved. Request academic re-use from www.copyright.com. All other uses, submit a request to [email protected]. For more information visit Asset & Logo Licensing.







