About The Author

CONNECT WITH THIS AUTHOR
March 06, 2025
March 22, 2024
November 15, 2022
Analysis
AARP's billion-dollar bounty
June 06, 2022
November 11, 2021
April 22, 2020
March 10, 2020
October 23, 2019
Market Insights
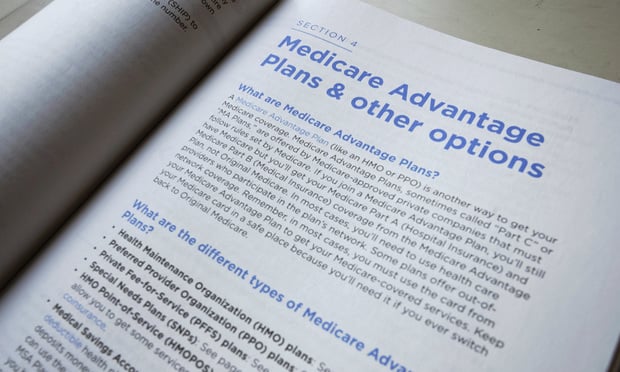
Taxpayers overpaying billions for Medicare Advantage
July 16, 2019
Trending Stories
- 1Enterprise ICHRA: A Playbook for Benefits Advisors
- 29 in 10 Americans have put off health checkups, life-saving screenings
- 3Willis Towers Watson sees tariff turbulence adding demand for health benefits advice
- 4Pharmacist group tells Elon Musk's team to probe pharmacy benefit managers
- 5Bank employees win $38M in Pentegra’s multiemployer 401(k) excessive fees case